-
by admin
IUD (intrauterine device, coil)
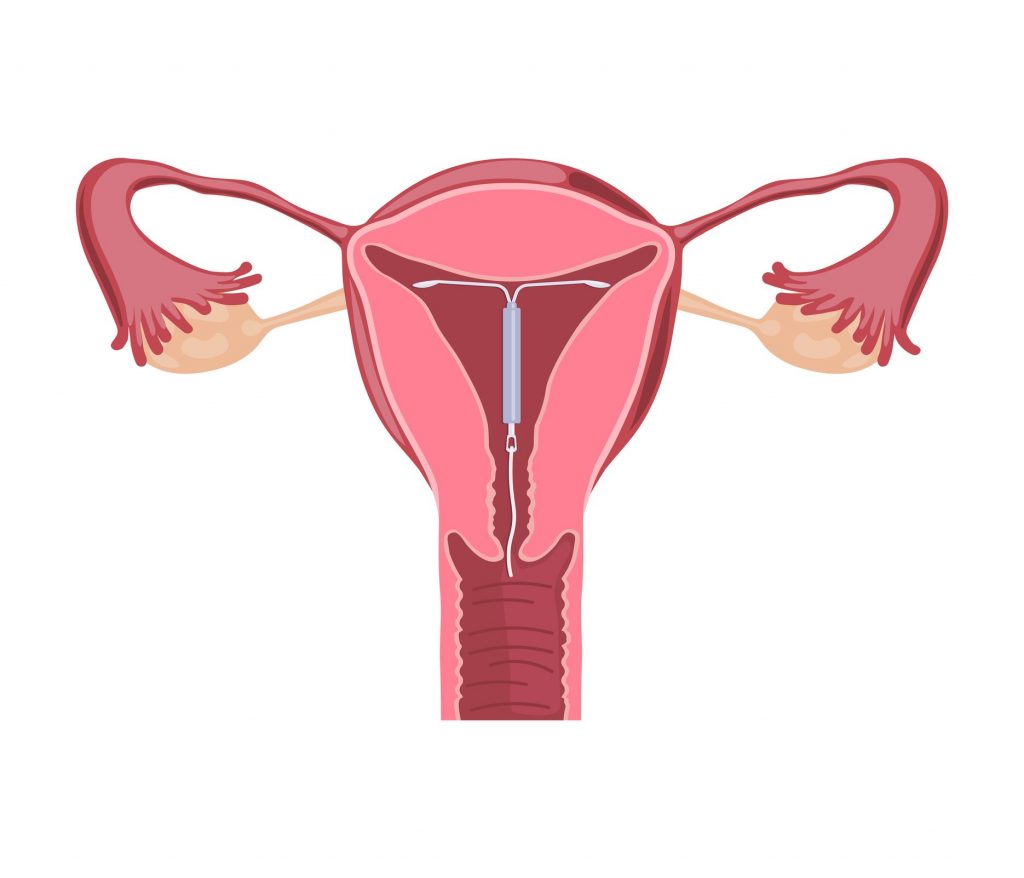
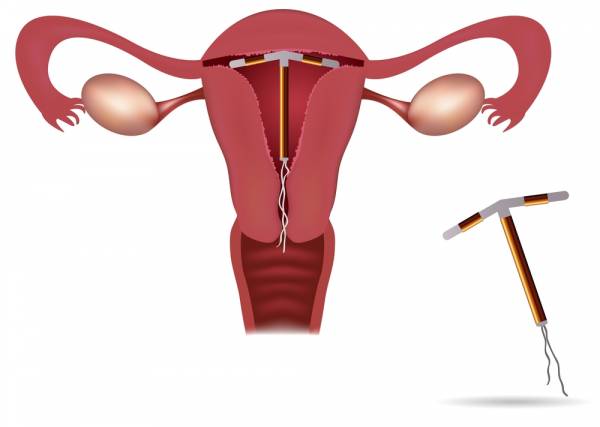
An IUD is a small T-shaped plastic and copper device that’s inserted into your womb (uterus) by a specially trained doctor or nurse.
The IUD works by stopping the sperm and egg from surviving in the womb or fallopian tubes. It may also prevent a fertilized egg from implanting in the womb.
The IUD is a long-acting reversible contraceptive (LARC) method. This means that once it’s in place, you don’t have to think about it each day or each time you have sex. There are several types and sizes of IUDs.
You can use an IUD whether or not you’ve had children.
At a glance: facts about the IUD
- There are different types of IUD, some with more copper than others. IUDs with more copper are more than 99% effective. This means that fewer than one in 100 women who use an IUD will get pregnant in one year. IUDs with less copper will be less effective.
- An IUD works as soon as it’s put in, and lasts for five to 10 years, depending on the type.
- It can be put in at any time during your menstrual cycle, as long as you’re not pregnant.
- It can be removed at any time by a doctor or nurse and you’ll quickly return to normal levels of fertility.
- Changes to your periods (for example, being heavier, longer or more painful) are common in the first three to six months after an IUD is put in, but they’re likely to settle down after this. You might get spotting or bleeding between periods.
- There’s a very small chance of infection within 20 days of the IUD being fitted.
- There’s a risk that your body may expel the IUD.
- If you get pregnant, there’s an increased risk of (when the egg implants outside the womb). But because you’re unlikely to get pregnant, the overall risk of ectopic pregnancy is lower than in women who don’t use contraception.
- Having the IUD put in can be uncomfortable. Ask the doctor or nurse about pain relief.
- An IUD may not be suitable for you if you’ve had previous pelvic infections.
- The IUD does not protect against sexually transmitted infections (STIs). Use condoms as well as the IUD, to protect yourself against STIs.
How an IUD works
The IUD is similar to the IUS (intrauterine system) but works in a different way. Instead of releasing the hormone progestogen like the IUS, the IUD releases copper. Copper changes the make-up of the fluids in the womb and fallopian tubes, stopping sperm from surviving there. IUDs may also stop fertilized eggs from implanting in the womb.
There are types and sizes of IUDs to suit different women. IUDs need to be fitted by a doctor or nurse at your GP surgery or sexual health clinic.
An IUD can stay in the womb for five to 10 years, depending on the type. If you’re 40 or over when you have an IUD fitted, it can be left in until you reach menopause or until you no longer need contraception.
Having an IUD fitted
An IUD can be fitted at any time during your menstrual cycle, as long as you are not pregnant. You’ll be protected against pregnancy straight away.
Before you have an IUD fitted, you will have an internal examination to find out the size and position of your womb. This is to make sure that the IUD can be put in the correct place.
You may also be tested for infections, such as STIs. It’s best to do this before an IUD is fitted so that you can have treatment (if you need it) before the IUD is put in. Sometimes, you may be given antibiotics at the same time as the IUD is fitted.
The fitting process can be uncomfortable and sometimes painful. You may get cramps afterward. You can ask for a local anesthetic or painkillers before having the IUD fitted. An anesthetic injection itself can be painful, so many women have the procedure without.
You may get pain and bleeding for a few days after having an IUD fitted. Discuss this with your doctor or nurse beforehand.
The IUD needs to be checked by a doctor after three to six weeks. Speak to your doctor or nurse if you have any problems before or after this first check or if you want the IUD removed.
Speak to your doctor or nurse if you or your partner are at risk of getting an STI. This is because STIs can lead to an infection in the pelvis.
See your GP or go back to the clinic where your IUD was fitted as soon as you can if you:
- have pain in your lower abdomen
- have a high temperature
- have a smelly discharge
This may mean you have an infection. You should also speak to your GP if you think your pregnant.
How to tell whether an IUD is still in place
An IUD has two thin threads that hang down a little way from your womb into the top of your vagina. The doctor or nurse who fits your IUD will teach you how to feel for these threads and check that it’s still in place.
Check your IUD is in place a few times in the first month, and then after each period or at regular intervals.
It’s very unlikely that your IUD will come out, but if you can’t feel the threads, or if you think the IUD has moved, you may not be fully protected against getting pregnant. See your doctor or nurse straight away and use an extra method of contraception, such as condoms, until your IUD has been checked.
Your partner shouldn’t be able to feel your IUD during sex. If he can feel the threads, get your doctor or nurse to check that your IUD is in place. They may be able to cut the threads to a shorter length. If you feel any pain during sex, go for a check-up.
Removing an IUD
An IUD can be removed at any time by a doctor or nurse.
If you’re not going to have another IUD put in and you don’t want to get pregnant, use another method (such as condoms) for seven days before you have the IUD removed. This is to stop sperm from getting into your body. Sperm can live for up to seven days in the body and could make you pregnant once the IUD is removed.
As soon as an IUD is taken out, your normal fertility should return.