-
by admin
Cap/Diaphragm
A woman can get pregnant if a man’s sperm reaches one of her eggs (ova). Contraception tries to stop this from happening by keeping the egg and sperm apart or by stopping egg production. One method of contraception is the cap.
Contraception tries to stop this from happening by keeping the egg and sperm apart or by stopping egg production.
The contraceptive cap is a circular dome made of thin, soft silicone. It’s inserted into the vagina before sex and covers the cervix so that sperm cannot get into the womb. You need to use spermicide with it (spermicide kills sperm).
The cap must be left in place for six hours after sex. After that time, you take out the cap and wash it. Caps are reusable. They come in different sizes, and you must be fitted for the correct size by a trained doctor or nurse.

At a glance: facts about the cap
- There’s one type of cap on the market in the UK just now: Femcap.
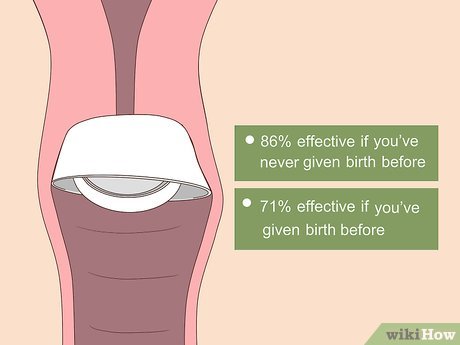
- There aren’t many studies of Femcap. It’s generally thought that when used correctly with spermicide, the cap is 92-96% effective at preventing pregnancy. This means that between four and eight women out of every 100 who use a cap as contraception will become pregnant in a year.
- As humans make mistakes, in real world use at least 12 women in 100 a year become pregnant (88% effective).
- There are no serious health risks of using the cap.
- A cervical cap can be inserted with spermicide any time before intercourse.
- You should use more spermicide if the cap has been in place for 3 hours or more, or if sex is repeated with the method in place.
- A diaphragm or cervical cap shouldn’t be removed until at least 6 hours after the last episode of intercourse.
- It can take time to learn how to use a cap.
- If you have a baby, miscarriage or abortion, you may need to be fitted with a new size of cap.
- By using condoms as well as a cap, you will help to protect yourself against.
How the cap works
A cap, like a diaphragm, is a barrier method of contraception. It fits inside your vagina and prevents sperm from passing through the entrance of your womb (the cervix). At present only one brand of cap is available in the UK, Femcap. Femcaps are soft, thin domes made of silicone, and come in three sizes.
About 80% of women find a Femcap that fits them. You can get a cap at some GP surgeries, sexual health clinics and some young people’s services.
To be effective in preventing pregnancy, the cap needs to be used in combination with spermicide, which is a chemical that kills sperm.
You only need to use a cap when you have sex. You must leave it in for at least six hours after the last time you have sex. You can leave it in for up to 48 hours.
For the best protection against STIs, it’s advised that you use a condom as well.
Inserting a contraceptive cap
Your doctor or nurse will show you how to put in a cap. Caps come with instructions and are all inserted in a similar way:
- With clean hands, fill one-third of the cap with spermicide, but do not put any spermicide around the rim, as this will stop the cap staying in place.
- Femcap has a groove between the dome and the rim – some spermicide should also be placed there.
- Squeeze the sides of the cap together and hold it between your thumb and first two fingers.
- Slide the cap into your vagina, upwards.
- The cap must fit neatly over your cervix – it stays in place by suction.
- Some women squat while they put their cap in, while others lie down or stand with one foot up on a chair – use the position that’s easiest for you.
- You can insert a cap up to three hours before you have sex – after this time, you will need to take it out and put some more spermicide on it.
When you are fitted with a cap you will be asked to practice with at home. This gives you the chance to learn how to use it properly, see how it feels and find out if the method is suitable for you. Until you are confident you’re using the cap correctly, you might need to use additional contraception, such as condoms, when you have sex.
When you go back for a follow-up appointment with your doctor or nurse, wear the cap so they can check that it is the right size and you have put it in properly.
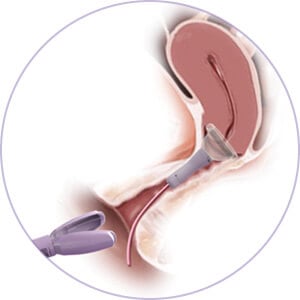
Removing a Femcap
A Femcap can be easily removed by gently hooking your finger under its rim, loop or strap and pulling it downwards and out. You must leave your cap in place for at least 6 hours after the last time you had sex. Sperm can survive up to 6 hours in the vagina so if the barrier is removed too early, you increase your chances of pregnancy.
You can leave a Femcap in for longer than this, but don’t leave it in for longer than the recommended maximum time of 48 hours.
Looking after your cap
After use, you can wash your cap with warm water and mild, unperfumed soap. Rinse it thoroughly, then leave to dry. You will be given a small container for it, which you should keep in a cool, dry place.
- Never boil a cap.
- Your cap may become discoloured over time, but this doesn’t make it less effective.
- Always check your cap for any signs of damage before using it.
You can visit your GP or nurse when you want to replace your cap. Most women can use the same cap for a year before they need to replace it. You may need to get a different sized cap if you have a baby, miscarriage or abortion.
Who can use the cap
Most women are able to use contraceptive caps. However, they may not be suitable for you if you:
- have an unusually shaped or positioned cervix (entrance to the womb), or if you cannot reach your cervix
- have a sensitivity or an allergy to the chemicals in spermicide
- have ever had toxic shock syndrome (a rare, but life-threatening bacterial infection)
- currently have a vaginal infection (wait until your infection clears before using a diaphragm or cap)
- are not comfortable touching your vagina
Research shows that spermicides that contain the chemical nonoxynol-9 do not protect against STIs and may even increase your risk of getting an STI. If you’re at a high risk of getting an STI, for example, if you have multiple sexual partners, a cap may not be the best choice for you.
A cap may be less effective if:
- it is damaged – for example, it is torn or has holes
- it is not the right size for you
- you use it without spermicide
- you do not use extra spermicide with your cap every time you have more sex
- you remove it too soon (less than six hours after the last time you had sex)
You can use a cap after having a baby, but you may need a different size. It is recommended that you wait at least six weeks after giving birth before using a contraceptive cap. You can use a cap after a miscarriage or abortion, but you may need a different size.
Advantages and disadvantages of the cap
A cap has the following advantages:
- you only need to use it when you want to have sex
- you can put it in at a convenient time before having sex (do not forget to use extra spermicide if you have it in for more than three hours)
- there are no serious associated health risks or side effects
A cap has the following disadvantages:
- it is not as effective as other types of contraception
- it only provides limited protection against STIs
- it can take time to learn how to use a cap
- putting a cap in can interrupt sex
- cystitis (bladder infection) can be a problem for some women who use a cap
- spermicide can cause irritation in some women and their sexual partners
Risks of the cap
There are no serious health risks associated with using a contraceptive cap.
Where you can get the cap?
Most types of contraception are free in the UK. Contraception is free to all women and men through the NHS. Places where you can get contraception to include:
- most GP surgeries – talk to your GP or practice nurse
- sexual health clinics – they also offer contraceptive and STI testing services
- some young people’s services
Contraception services are free and confidential, including for people under the age of 16.
If you’re under 16 and want contraception, the doctor, nurse or pharmacists won’t tell your parents (or carer). They will provide you with contraception as long as they believe you fully understand the information you’re given and are able to use the contraception safely.
Doctors and nurses have a responsibility to make sure that you are safe and free from harm. They’ll encourage you to consider telling your parents (or carer), but they won’t make you. The only time that a professional will not be able to keep confidentiality is if they believe you’re at risk of serious harm, such as abuse. If this was the case they would usually discuss it with you first.